Friday was a very quiet day. In the morning, we had four optoms working but only enough patients for two of the four. I spent the first couple of hours of the day catching up on little things, cleaning my equipment and obsessively updating the diary on my computer to see if there were any walk-ins.
Around mid-morning, we started to get a little busier. First a young girl who was struggling with the board at school. Then there was a mature student who wanted to know about Meares-Irlen (I spent far too long chatting to her and sharing my experience of being tested for visual stress). Then we had a woman my age with a severe headache.
The woman (J) had been to the GP that morning and the doctor had told her to go to an optician as soon as possible. He had mentioned her optic discs. J looked like she was having a migraine. Her lids were heavy and she was tired. I could see she was struggling with this headache.
During H&S, I followed the LOFTSEA approach:
1) Location – frontal, right hand side, moving down the face.
2) Onset – the headaches started 3 weeks ago, on and off, but the latest one had lasted three days (and she was still suffering with it, even although her GP had given her some hefty painkillers).
3) Frequency – almost every day but each one can last days.
4) Type – this was difficult. She couldn’t describe the pain, except that it was intense. It wasn’t an ache or a pressure, it wasn’t sharp or dull. It was just painful.
5) Severity – very severe. So much so that she’d been sent home from work.
6) Effectiveness of remedies – the painkillers had taken the edge off but she was still in pain.
7) Associated factors – she was nauseated as well, especially when looking down.
IOPs were within the normal range and she wore distance specs (her Rx was mainly astigmatism).
After history and symptoms, I check unaided vision. She was 6/6 and N5 without her specs. I then did cover test – no movement. Then pupils. Then pupils again. And then more pupils. For those of you who haven’t seen an RAPD and worry about missing one then don’t: as long as you are paying attention, you’ll notice something is wrong.
J had noticeable anisocoria but I really wasn’t expecting the RAPD. When I swung the pen torch over from the constricting right pupil to her left eye, the left eye dilated. There wasn’t that usual momentary flicker of dilation followed by constriction, the left eye went from miosed to fully dilated when the light was shining into it. In short: it looked weird.
At this point I asked J if she wanted to have a full eye test or I could just skip the refraction part and look in her eyes. She was adamant that she was fine having the full eye test, although I could see her struggling under this horrible headache.
Refraction was very straight forward. She came down to R 6/4 and L 6/5 with specs. While I was refracting, I kept asking myself if it could be papilloedema – surely her VA would be worse?
Confrontation fields were difficult as she kept looking towards my confrontation stick and then apologising.
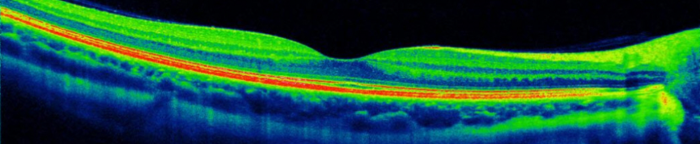
When I looked in her eyes, both discs looked indistinct. The left disc was definitely swollen but the right just looked a bit fuzzy. The blood vessels were tortuous in both eyes but with the left worse than the right. I spent a moment looking and comparing the discs (while doing Volk, I look at the disc in the RE first, then have a good look around, asking the px to look in the 8 directions of gaze and then, at the last moment, I return to the disc so that it’s fresh in my mind when I move over to the LE). I narrowed the beam and tried angling it slightly to gauge how raised both the discs were (this didn’t work).
Everything else looked healthy and normal.
I explained to J about the optic nerves in her eyes and how, if there is pressure from behind, they can become swollen. This, together with her headache, meant that I wanted to send her to the hospital straight away. I then asked her to wait outside while I called the ophthalmologist, who agreed to see J that afternoon, based on her symptoms. I then had to explain to J that it would be best if someone drove her to the hospital as they would instill drops and, on the ophthalmologist’s instructions, I also told her that they might want to keep her in hospital overnight.
After J left, I called and left a message for her GP saying that I’d referred J to hospital and that she was being seen that afternoon. I also sent him a copy of the referral letter but I thought the GP would like to know that his suspicions were correct and to thank him for sending her in to us.
I asked J to call me when she got home from the hospital but she hasn’t yet.